Conditions & Symptoms
Types of Thyroid Disease
How Does the Thyroid Gland Work?
What is the Prevalence of Thyroid Disease?
What is Hypothyroidism?
What is Hashimoto’s Thyroiditis?
What is Hyperthyroidism?
What is Graves’ Disease?
What is Thyroid Cancer?
Take the Symptoms Checklist to Your Doctor

Print the thyroid disease symptom checklist by Holtorf Medical Group! This can be easily completed and then presented to your doctor. Symptom assessment is a vital part of proper diagnosis and treatment. This tool can help you when discussing the number of symptoms you have with your doctor.
How Does the Thyroid Gland Work?
The endocrine system is a network of glands, including the thyroid, which secrete various hormones into the bloodstream, helping to regulate the function of various tissues and organs. The thyroid is butterfly-shaped with symmetrical lobes that wrap around your trachea, just below the ‘Adam’s apple’. This gland is responsible for the production and secretion of thyroid hormones that play a major role in your body’s metabolism [1].
Know Your Thyroid Hormones
The most important thyroid hormones that you will hear discussed are T4, T3, and Reverse T3 (RT3). The thyroid uses iodine and other molecules to create these hormones, including T1, T2, and calcitonin, too.

T4 (thyroxine)
Inactive ‘storage’ hormone that converts to either T3 or Reverse T3.

T3 (triiodothyronine)
Active hormone which is needed by every cell and is either made by the thyroid or converted in the body.

Reverse T3 (reverse triiodothyronine)
Inactive conversion hormone of T4. Serves as the ‘brakes’ of T3 by inhibiting T3 production or blocking receptor sites.
How Are They Produced?
It’s important to know how the thyroid hormones are produced and work together in your body since a dysfunction or imbalance can happen in any one of the following steps:
STEP 1
The hypothalamus gland in the brain releases thyrotropin-releasing hormone (TRH) when it senses the body needs thyroid hormone.
STEP 2
TRH signals the pituitary gland in the brain to secrete thyroid stimulating hormone (TSH).
STEP 3
TSH stimulates the thyroid gland to produce thyroid hormones including both T4, the “storage” hormone, and T3, the active hormone.
STEP 4
T4 is then converted into T3 hormone and Reverse T3by deiodinase enyzmes. This mainly occurs in the liver.
STEP 5
Proteins produced by the liver, such as thyroid binding globulin (TBG), carry the T3 hormone to the tissues where they bind to thyroid hormone receptors (THRs) and interact with your cells [41].
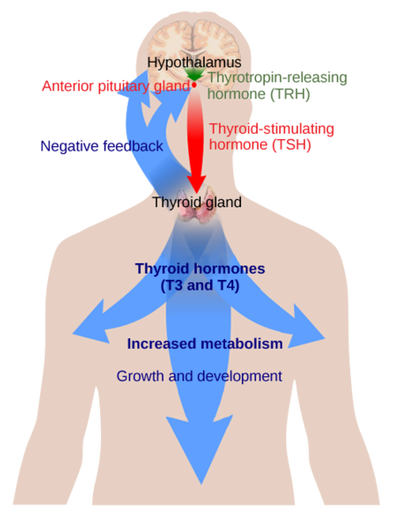
How Do They Affect Your Body?
This vast hub of communication, known as the hypothalamic–pituitary–thyroid (HPT) axis, is a sensitive feedback loop which controls one of the most fundamental needs of your body: sufficient thyroid hormone for every cell [3]. The HPT axis controls the delicate production of thyroid hormones and how they work together to achieve balance. For instance, too much or too little T3 can speed up or slow down body processes, from the rate of your heartbeat, to how food passes through your system, to the speed of cell regeneration [2]. And for instance, the presence of too much or too little RT3 affects T3 action; and T4 (the storage hormone), needs to be converted properly to maintain proper levels of the most biologically active hormone, T3.
Implications For Testing and Treatment
HPT axis process is the basis for the standard reliance on the TSH laboratory test for the detection of thyroid disease. However, TSH is not the only factor in producing healthy thyroid hormone levels and receptivity. Numerous processes in the body can interrupt the feedback loop. A full thyroid panel is recommended by many practitioners to assess the levels of thyroid storage hormone or active hormone that is available to the cells [24-30]. Additionally, a problem converting T4 to T3, or a problem with cellular thyroid resistance may warrant treatment options beyond T4-only medication (e.g. levothyroxine). Such options include combination T3/T4 medication, desiccated thyroid extract, or T3-containing medication such as liothyronine [42].
How Common Is Thyroid Disease?
These statistics are startling and should serve as a reminder to patients and doctors alike. Undiagnosed thyroid disease is more common than we think, and women are at a higher risk and should be carefully monitored for the presentation of thyroid conditions.
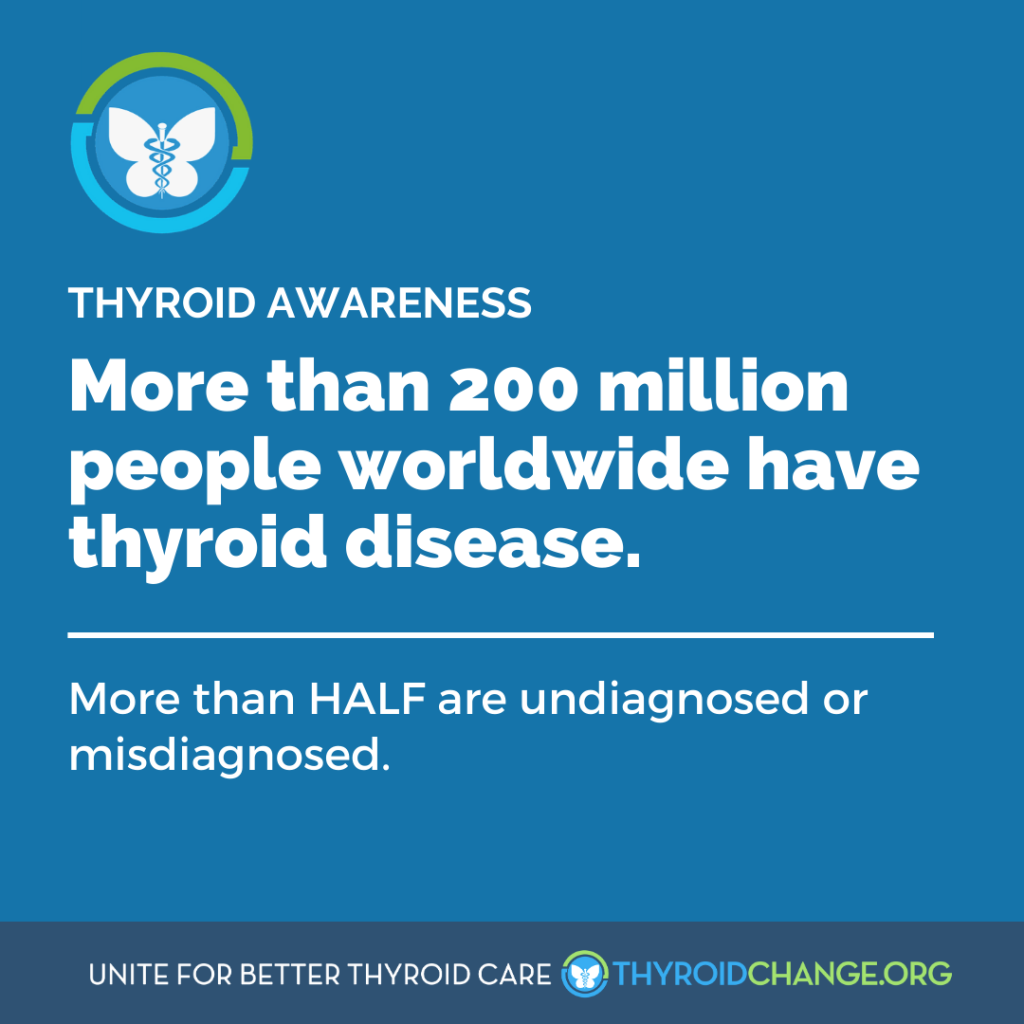
- Thyroid disease is more common than diabetes or heart disease as reported by the AACE.
- The AACE estimates as many as 30 million Americans have thyroid disease.
- Approximately, 15 million of those individuals are undiagnosed and are walking at risk and unaware.
- There is a strong genetic link between thyroid disease and other autoimmune diseases, including diabetes, arthritis and anemia, as well as a risk for other diseases [5].
- Women are seven times more likely than men to suffer from hypothyroidism (a deficiency in thyroid hormone) [5].
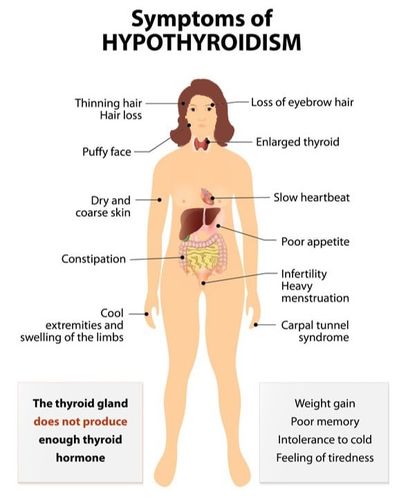
What Is Hypothyroidism?
Hypothyroidism is a condition where there is not enough thyroid hormone for the body to function properly. Since every cell needs thyroid hormone for its essential function, insufficient thyroid hormone will affect every function of the human body [8]. A common symptom of hypothyroidism is the slowing of metabolism which often results in weight gain. It also affects numerous body systems including digestion, the central nervous system, the cardiovascular system, the pulmonary system, the skin, hair growth, vision, musculature, fetal development, the reproductive system, and bone growth [9].
Worldwide, the most common cause of hypothyroidism is iodine depletion. However, in those countries with sufficient iodine in their food sources such as the United States, an autoimmune disease called Hashimoto’s thyroiditis causes over 90% of hypothyroidism [10]. This disorder causes a patient’s body to create antibodies which attack and slowly destroy the thyroid gland, eventually preventing the thyroid from being able to create enough hormone for proper functioning [11].
There are many other factors that can cause hypothyroidism such as medications, chronic illness, hormonal changes, pregnancy, menopause and aging [8]. High levels of Reverse T3 can cause cellular hypothyroidism. The action of Reverse T3 will both block T3 cellular receptor sites and inhibit conversion of T4 to T3. Therefore, high Reverse T3 and low T3 will create insufficient active T3 at the cellular level, also called Low T3 Syndrome. [4]. Patients must work with their doctors to identify symptoms and to run proper laboratory testing for thyroid hormone evaluation.
What Are the Signs and Symptoms of Hypothyroidism?
Each person is unique. Hypothyroidism can present itself differently in many patients with a range of symptoms that can vary in severity. Lack of sufficient thyroid hormone affects every body system and there are hundreds of symptoms reported throughout the patient population [8]. It must be noted that all symptoms of thyroid disease do not need to exist to receive a diagnosis. The following symptoms have been identified as the most common in hypothyroidism [12]:
- Weight gain
- Fatigue
- Low body temperature
- Depression/anxiety
- Slow movements, thought and speech
- Breathlessness
- Tingling sensations
- Dizziness
- Palpitations
- Loss of libido
- Dry/gritty eyes
- Hoarse voice
- Difficulty swallowing
- Hair loss; especially outer third of eyebrows
- Dry skin
- Muscle and joint pain
- Loss of appetite
- Constipation
- Fertility or menstrual issues
Visit the downloadable thyroid disease symptom checklist by Holtorf Medical Group that can be presented to your physician.
For information about diagnostic methods and testing, please visit here.
For effective treatment options, please visit here.
What is Hashimoto’s Thyroiditis?
Hashimoto’s thyroiditis is an autoimmune disease that is also known as Hashi’s, chronic lymphocytic thyroiditis, and autoimmune thyroiditis. It is the most common cause of thyroid disease in the Western world affecting .1 to 5% of all adults [12].
In Hashimoto’s thyroiditis, the body creates antibodies which attack thyroid tissue causing inflammation which prevents the thyroid from effectively producing hormones.
Many individuals with Hashimoto’s will be rendered hypothyroid for life and will need thyroid hormone replacement to restore their health. Patients may not be aware of the onset of Hashimoto’s due to its progressive nature and may have increasing symptoms over time [16].
Many physicians treat Hashimoto’s with thyroid replacement only after the patient’s lab report reveals hypothyroidism.
However, mounting evidence and physician reports suggest that patient symptom report along with elevated thyroid antibody levels is grounds for treatment. If Hashimoto’s thyroiditis is not treated there can be many complications.
Since it results in the underproduction of thyroid hormone, please see “What Are the Signs and Symptoms of Hypothyroidism?” listed above for common symptoms. Additionally, due to the antibody attack, a patient’s thyroid may swell causing a goiter. A goiter can become uncomfortable and cause a choking sensation for the individual. Furthermore, myxedema is also a risk for untreated Hashimoto’s patients. It is a condition that can cause a coma due to the stress on the body from insufficient thyroid hormone [11]. Women are more likely to have Hashimoto’s and as a result, are at higher risk for preeclampsia, anemia, miscarriage, placental abruption, and postpartum bleeding. Additionally, untreated Hashimoto’s increases an infant’s risk of pre-term birth, low birth weight, still-birth and thyroid disorders [16]. Therefore, a woman’s thyroid antibody status is significant to her pregnancy success and should be considered a vital evaluation when preparing to conceive.Visit the downloadable thyroid disease symptom checklist by Holtorf Medical Group that can be presented to your physician.
For information about diagnostic methods and testing, please visit here.
For effective treatment options, please visit here.
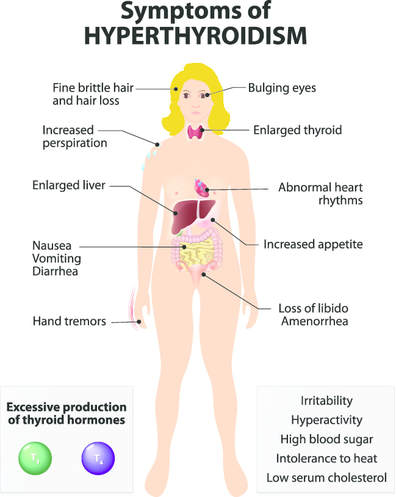
What Is Hyperthyroidism?
The opposite of the slowing effect of insufficient thyroid hormone is the acceleration of body processes from excess thyroid hormone known as hyperthyroidism. Hyperthyroidism puts a patient at risk for thyrotoxicosis which refers to high levels of thyroid hormone regardless of origin. Thyrotoxicosis can be toxic, therefore careful monitoring must be in place when hyperthyroidism is diagnosed or when it is being treated.
Similar to hypothyroidism, there are many causes for a hyperthyroid state. The most common is an autoimmune disease called Graves’ disease which is the cause of hyperthyroidism in eighty percent of cases [21]. In Graves’ disease, antibodies produced by the immune system stimulate the thyroid gland to produce too much T4. Other causes of hyperthyroidism are hormonal changes during the postpartum period, toxic multi-nodular goiter, toxic adenoma, Hashimoto’s (patients can be hyperthyroid at times), pituitary problems, over-medication with thyroid hormones and rarely, cancer. Hyperthyroidism occurs in one percent of Americans. Women have five to ten times the risk that men have [22].
An excess of iodine may cause hyperthyroidism. The thyroid gland uses iodine to make thyroid hormones. When there is an excess of iodine, overproduction of thyroid hormone can occur. People who consume too much iodine (either from food or supplements) or who take medications containing iodine, such as the heart medication amiodarone, may be at risk for over-producing thyroid hormones, leading to hyperthyroidism [31].
As mentioned, a toxic nodular or multi-nodular goiter may also cause hyperthyroidism. A toxic nodular or multi-nodular goiter are lumps or nodules in the thyroid gland that cause the thyroid to produce excessive amounts of thyroid hormones. Additionally, thyroiditis (or inflammation of the thyroid gland) resulting from chronic infection or a problem with the immune system may also cause symptoms of hyperthyroidism [32].
What Are the Signs and Symptoms of Hyperthyroidism?
Hyperthyroidism can affect many patients differently and can cause a wide range of symptoms of varied severity from head to toe. An overabundance of sufficient thyroid hormone affects every body system and there can be hundreds of symptoms [9]. It must be noted that all symptoms of thyroid disease do not need to exist in order to get a proper diagnosis. The most common symptoms are listed below:
- Nervousness/Anxiety
- Goiter – swollen thyroid
- Increased appetite
- Weight loss despite healthy diet; increased appetite
- Bloodshot whites of eyes; gritty feeling
- Irregular or fast heart rate
- Loose bowel movements, fast digestion
- Shortness of breath
- Intolerance to heat
- Increased sweat production
- Inability to sleep [23]
Visit the downloadable thyroid disease symptom checklist by Holtorf Medical Group that can be presented to your physician.
For information about diagnostic methods and testing, please visit here.
For effective treatment options, please visit here.
What is Graves’ Disease?
Graves’ disease is the cause for eighty percent of all hyperthyroid cases. It is an autoimmune disease where the immune system makes antibodies that act like TSH, causing the thyroid to make more thyroid hormone than the body needs. This is called an overactive thyroid or hyperthyroidism. An overactive thyroid causes every function of the body to speed up, such as heart rate and metabolism. Women are more at risk for Graves’ than men and women of childbearing age must take caution since Graves’ is associated with greater risk of miscarriage and a greater risk for birth defects.
Many factors are thought to play a role in a person developing Graves’ disease. Since it is an autoimmune disease, certain triggers can cause an antibody attack such as stress, sex hormone imbalances, infection, and allergies. Additionally, there is a genetic component with Graves’ disease and patients with a family history of autoimmune thyroid disease are more likely to have it. Exactly why the immune system begins to produce these antibodies is unclear. Without treatment, Graves’ disease can lead to heart problems, weak and brittle bones. A ‘thyroid storm’ can develop if an overactive thyroid is not treated. While a “thyroid storm” is a rare condition of extreme hyperthyroid symptoms, it can be life-threatening [33].
Eye trouble can be a complication of Graves’ disease. Some patients may experience inflamed and swollen eye muscles and tissues than can cause the eye to protrude from their sockets. This is known as exophthalmos and occurs in only a small percentage of all Graves’ patients. In severe cases of exophthalmos, the swollen eye muscles can place pressure on the optic nerve, which could possibly lead to blindness. Additionally, double vision can occur if the eye muscles are weakened by long periods of inflammation and lose their ability to control movement [34].
Since Graves’ disease results in the overproduction of thyroid hormone, please see “What Are the Signs and Symptoms of Hyperthyroidism?” that is listed above for common symptoms.
Visit the downloadable thyroid disease symptom checklist by Holtorf Medical Group that can be presented to your physician.
For information about diagnostic methods and testing, please visit here.
For effective treatment options, please visit here.
What is Thyroid Cancer (Thyroid Carcinoma)?
Thyroid cancer occurs when cells in your thyroid undergo genetic changes or mutations. The mutations allow the cells to grow and multiply rapidly. The cells lose their ability to die, as normal cells would. The accumulating malignant cells form a tumor. These abnormal cells can invade nearby tissue and spread throughout the body [35]. Thyroid cancer is more common in women than in men. Most patients who are diagnosed with thyroid cancer are between 25 and 65 years old [38].
It is not clear what causes thyroid cancer, but as with other cancers, changes in the DNA of cells seem to play a role. These DNA changes may be inherited changes as well as changes that can happen as a person gets older [37]. People who have been exposed to large amounts of radiation, or who have had radiation treatment for medical problems in the head and neck have a higher chance of being diagnosed with thyroid cancer [38].
What Are the Signs and Symptoms of Thyroid Cancer?
Thyroid cancer can cause several symptoms, however, some people may not have any symptomatic manifestations. Their doctors may find a lump or nodule in the neck during a routine physical exam which would then call for further testing [37]. Any of the following symptoms can be reported:
- Lump or nodules in the front of the neck
- Swelling of the neck
- Enlarged lymph nodes in front of the neck
- Problems with swallowing
- Hoarseness or voice changes
- Pain or discomfort in the neck and/or ears
- Trouble breathing or constant wheezing
- Chronic cough

What are the Types of Thyroid Cancer?
There are several types of thyroid cancer:
- Papillary: In the United States, papillary thyroid cancer is the most common type. About 86 of every 100 people with thyroid cancer have this type. It begins in follicular cells and usually grows slowly. If diagnosed early, most people with papillary thyroid cancer can reach remission.
- Follicular: The second most common type is follicular thyroid cancer. A little more than 9 of every 100 people with thyroid cancer have this type. It begins in follicular cells and usually grows slowly. If diagnosed early, most people with follicular thyroid cancer can reach remission.
- Medullary: Medullary thyroid cancer is not common. About 2 of every 100 people with thyroid cancer have this type. It begins in C cells and can make abnormally high levels of calcitonin. Medullary thyroid cancer tends to grow slowly. Medullary thyroid cancer sometimes runs in families.
- Anaplastic: The least common type is anaplastic thyroid cancer. About 1 of every 100 people with thyroid cancer has this type. Most people with anaplastic thyroid cancer are older than 60. The cancer begins in follicular cells of the thyroid. The cancer cells tend to grow and spread very quickly. Anaplastic thyroid cancer is very difficult to control [36].
If diagnosed and treated early, thyroid cancer treatment can be highly effective and usually includes the surgical removal of a portion or the entire thyroid gland, and perhaps, treatment with a form of radiation such as radioactive iodine (RAI), also known as I-131 [39]. Following surgery or RAI, the patient is often considered hypothyroid and can begin thyroid hormone replacement therapy as described above.
Due to the individual nature of cancer staging and treatment, patients must work closely with their doctors to create an individualized treatment plan. It is highly recommended that the patient finds a surgeon skilled in thyroid gland removal to minimize complications such as collateral damage to the parathyroid glands. The effectiveness of thyroid cancer treatment lends itself to the reputation of being a “good cancer” to have, however, it should not be minimized and needs effective treatment and monitoring.
For more information regarding types and stages of thyroid cancer, please see the ThyCa website.Visit the downloadable thyroid disease symptom checklist by Holtorf Medical Group that can be presented to your physician.
For information about diagnostic methods and testing, please visit here.
For effective treatment options, please visit here
References
1. PubMed Health. “How does the thyroid gland work?” http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0010393/
2. Endocrine Web. How your thyroid works: A delicate feedback mechanism”. www.endocrineweb.com/conditions/thyroid/how-your-thyroid-works
3. AACE Empower Your Health. “About your thyroid”. http://empoweryourhealth.org/Overactive-Thyroid
4. Mayo Medical Laboratories. http://www.mayomedicallaboratories.com/test-catalog/Clinical+and+Interpretive/9405
5. AACE Empower Your Health. “About Hashimoto’s thyroiditis”. http://empoweryourhealth.org/endocrine-conditions/thyroid/about_hashimotos_thyroiditis
6. Thyroid Cancer Survivors’ Association, Inc. “Facts about thyroid cancer”. :http://www.thyca.org/about/thyroid-cancer-facts
7. Healthy Women. “Thyroid disorders”. http://www.healthywomen.org/condition/thyroid-disorders
8. AACE Empower Your Health. “What is hypothyroidism?”. http://empoweryourhealth.org/endocrine-conditions/thyroid/about_hypothyroidism
9. Hypothyroid Mom. ‘300+ hypothyroidism symptoms…yes, really” https://hypothyroidmom.com/300-hypothyroidism-symptoms-yes-really
10. American Thyroid Association. “FAQ: Hypothyroidism”. http://www.thyroid.org/faq-hypothyroidism/
11. Mayo Clinic. “Hashimoto’s disease“. http://www.mayoclinic.org/diseases-conditions/hashimotos-disease/basics/definition/con-20030293
12. Thyroid UK. “Hypothyroidism”. http://www.thyroiduk.org.uk/tuk/about_the_thyroid/hypothyroidism.html
13. U.S. National Library of Medicine. “Chronic thyroiditis: Hashimoto’s disease”. http://www.nlm.nih.gov/medlineplus/ency/article/000371.htm
14. Takami, Hiroshi E., Rika Miyabe, and Kaori Kameyama. “Hashimoto’s thyroiditis.” World journal of surgery 32.5 (2008): 688-692.
http://www.ncbi.nlm.nih.gov/pubmed/18305995
15. UCSF Diabetes Education Online. “What causes autoimmune diabetes?”. http://dtc.ucsf.edu/types-of-diabetes/type1/understanding-type-1-diabetes/autoimmunity/what-causes-autoimmune-diabetes/
16. Office on Women’s Health. “Hashimoto’s disease fact sheet”. http://www.womenshealth.gov/publications/our-publications/fact-sheet/hashimoto-disease.html
17. Medline Plus. “Autoimmune diseases”. http://www.nlm.nih.gov/medlineplus/autoimmunediseases.html
18. Orrù, Valeria, et al. “Genetic variants regulating immune cell levels in health and disease.” Cell 155.1 (2013): 242-256.http://www.cell.com/abstract/S0092-8674%2813%2901072-6
19. Simons Foundation Autism Research Initiative. “Studies of early development reveal immune link to autism”. http://sfari.org/news-and-opinion/news/2011/studies-of-early-development-reveal-immune-link-to-autism
20. Mayo Clinic. “Hyperthyroidism (Overactive thyroid)”. http://www.mayoclinic.org/diseases-conditions/hyperthyroidism/basics/definition/con-20020986
21. Thyroid UK. “Hyperthyroidism – The Overactive Thyroid”. http://www.thyroiduk.org.uk/tuk/about_the_thyroid/hyperthyroidism.html
22. AACE Empower Your Health. “What is hyperthyroidism?”. http://empoweryourhealth.org/endocrine-conditions/thyroid/about_hyperthyroidism
23. Medline Plus. “Hyperthyroidism”. http://www.nlm.nih.gov/medlineplus/hyperthyroidism.html
24. Becker DV, Bigos ST, Gaitan E, Morris JC, Rallison ML, Spencer CA, Sugarawa M, Van Middlesworth L, Wartofsky L. Optimal use of blood tests for assessment of thyroid function. Journal of the American Medical Association. 1993 Jun 2; 269: 273.
25. Kalra S, Khandelwal, SK. Why are our hypothyroid patients unhappy? Is tissue hypothyroidism the answer? Indian Journal of Endocrinology and Metabolism. 2011 July; 15 (Suppl2): S95–S98.
26. Chopra IJ. Euthyroid sick syndrome: Is it a misnomer? Journal of Clinical Endocrinology and Metabolism. 1997; 82(2):329–34.
27. Schwartz E, Morelli V, Holtorf K. Hormone Replacement Therapy in the Geriatric Patient: Current State of the Evidence and Questions for the Future. Estrogen, Progesterone, Testosterone, and Thyroid Hormone Augmentation in Geriatric Clinical Practice. Clinics in Geriatric Medicine. 2011; 561–575.
28. De Los Santos ET, Mazzaferri EL. Sensitive thyroid-stimulating hormone assays:Clinical applications.Comprehensive Therapy.1988; 14(9): 26-33.
29. Alevizaki M, Mantzou E, Cimponeriu AT, Alevizaki CC, Koutras DA. TSH may not be a good marker for adequate thyroid hormone replacement therapy. Wiener klinische Wochenschrift. 2005; 117/18:636-640.
30. Nygaard, Birte, et al. Effect of combination therapy with thyroxine (T4) and 3, 5, 3′-triiodothyronine versus T4 monotherapy in patients with hypothyroidism, a double-blind, randomised cross-over study.”European Journal of Endocrinology 161.6 (2009): 895-902.
31. MedicineNet. “Hyperthyroidism”. http://www.medicinenet.com/hyperthyroidism/article.htm
32. Endocrine Web. “Hyperthyroidism Overview”. http://www.endocrineweb.com/conditions/hyperthyroidism/hyperthyroidism-overview-overactive-thyroid
33. Office on Women’s Health. “Graves’ Disease”. http://www.womenshealth.gov/publications/our-publications/fact-sheet/graves-disease.html
34. WebMD. “Graves’ Disease’. http://www.webmd.com/women/understanding-graves-disease-basics
35. Mayo Clinic. “Thyroid Cancer”. http://www.mayoclinic.org/diseases-conditions/thyroid-cancer/basics/definition/con-20043551
36. MedicineNet. “Thyroid Cancer”. http://www.medicinenet.com/thyroid_cancer/article.htm
37. WebMD. “What is Thyroid Cancer?” http://www.webmd.com/cancer/tc/thyroid-cancer-topic-overview
38. Thyca: Thyroid Cancer Survivor’s Association, Inc. “Thyroid Cancer Types, Stages, and Treatment Overview”. http://www.thyca.org/about/types/
39. National Cancer Institute: http://www.cancer.gov/cancertopics/wyntk/thyroid/page4
40. American Thyroid Association. “Goiter”. http://www.thyroid.org/what-is-a-goiter/
40. EmpowerHER.”What Are the Different Types of Thyroid Disease?” http://www.empowher.com/thyroid-conditions/content/what-are-different-types-thyroid-disease?page=0,1
41. Kresser, Chris. Low T3 Syndrome I: It’s Not About the Thyroid! Chris Kresser: Let’s Take Back Your Health. http://chriskresser.com/low-t3-syndrome-i-its-not-about-the-thyroid.
42. Baisier, W. V., J. Hertoghe, and W. Eeckhaut. Thyroid insufficiency. Is thyroxine the only valuable drug?. Journal of Nutritional and Environmental Medicine 11.3 (2001): 159-166.
DISCLAIMER: The information contained on the website and social media pages of ThyroidChange is for general information only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. ThyroidChange, Denise Roguz, guest writers, and partners are not responsible or liable for any advice or course of treatment that visitors choose to embark on. Please consult with your own health care practitioner regarding information or consults obtained through ThyroidChange or Denise Roguz. All material presented on this website is intended to be used for educational purposes only.